Swallowing problems are very common after a stroke. Almost half of people who have a stroke will have swallowing problems at first, but it often improves quickly. Watch our partner video about soft foods.
The information on this page can be accessed in the following formats:
- Download this information as a pdf or large print document.
- Order a printed copy from our shop
- To request a braille copy, email helpline@stroke.org.uk
On this page:
Why can't I swallow?
The four stages of swallowing
Can swallowing problems make you unwell?
Signs of swallowing problems.
Signs of complications due to swallowing problems.
Are there treatments that can help?
Changing how you eat and drink.
Swallowing assessments.
Tube feeding.
Tips for living with swallowing problems
Tips for family and friends
Why can't I swallow?
Swallowing is a complicated task that needs your brain to coordinate many different muscles. If your stroke damages the parts of your brain that do this, then this will affect your ability to swallow. Swallowing problems are also known as dysphagia.
Other effects of stroke can make eating, drinking and swallowing difficult too. If your arm or hand has been affected by your stroke, you may not be able to use a spoon or a cup properly. This can affect the way you swallow. If your face or lip muscles are affected, you might find that saliva escapes from your mouth
If your balance has been affected, you may not be able to sit up straight, which can make swallowing more difficult. If you're drowsy or not able to concentrate very well, then you may not swallow your food in the right way.
The four stages of swallowing
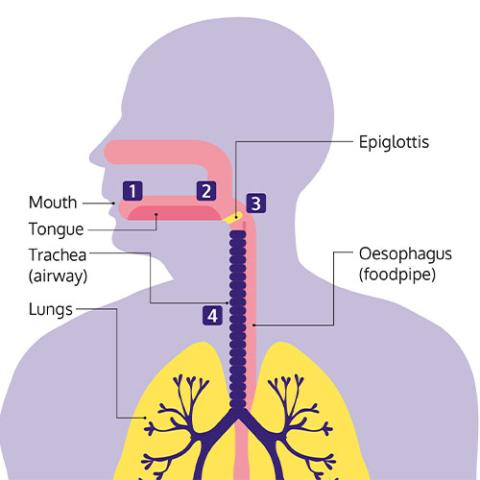
There are several stages to swallowing. A stroke can affect any one of these stages.
The four stages of swallowing:
- You see and smell food and put it in your mouth. You then prepare it for swallowing by chewing and moving it around your mouth.
- Your tongue moves the food or drink to the back of your mouth.
- The food or drink moves through your throat to your food pipe (oesophagus), which carries food to your stomach. At the point of swallowing, a flap in your throat (the epiglottis) moves to close over and protect your airway. This stops any food from going into your lungs.
- The muscles in your oesophagus squeeze in waves from top to bottom, moving the food down into your stomach.
Can swallowing problems make you unwell?
If you can't swallow correctly then food and drink may be getting into your airway and lungs. Saliva can also enter the airway if someone isn't able to swallow properly, or if they are drowsy and can't cough. This is called aspiration.
Aspiration can be very serious. Your mouth contains high numbers of bacteria (germs) and if these enter the airway, it can lead to pneumonia. So it's extremely important that any change to your swallowing is spotted early, to avoid this happening.
The stroke team watches carefully for any signs of aspiration and pneumonia.
Everyone who has a stroke should have their swallowing assessed within four hours of arriving at the hospital, and you shouldn't have any food, drink or medications by mouth until your swallowing has been assessed.
Signs of swallowing problems
Swallowing problems aren't always obvious, so it's good to know what to look out for. Signs of swallowing problems include:
- Coughing or choking when you're eating or drinking.
- Bringing food back up, sometimes through your nose.
- Food or drink going down the wrong way.
- Feeling that food is stuck in your throat.
- Not being able to keep food or drink in your mouth.
- Still having food or drink left in your mouth after you've swallowed.
- Not being able to chew food properly.
- A croaky or 'wet' sounding voice.
- Saliva escaping from your mouth.
- Taking a long time to swallow or finish a meal.
- Having to swallow a lot to clear your throat, or loudly clearing your throat.
- Being short of breath when you're swallowing.
Signs of complications due to swallowing problems
Lung infections (pneumonia)
After a stroke, your risk of a lung infection (pneumonia) is higher. Pneumonia can also be caused by coronavirus (Covid-19).
These are some of the main signs of pneumonia:
- High temperature, aches, and pains.
- A cough, sometimes with green or yellow phlegm.
- Difficulty breathing such as feeling out of breath, or rapid, shallow breathing.
- Chest pain
There are other signs of pneumonia, so check with a health professional or contact 111 if you notice any symptoms of infection. If someone is struggling to breathe or has chest pain or a rapid heartbeat, call 999. For more information about pneumonia, including a list of symptoms and advice on when to seek help, visit the NHS website.
Weight loss
Over time, swallowing problems can lead to you losing weight, or not getting enough nutrients from your diet. If you weigh less than usual, or you notice your clothes getting looser, speak to your dietitian, speech and language therapist, or stroke nurse. If you don't have a therapist, contact your GP.
You need to get enough energy (calories) and nutrients from your food, to help your body and brain recover after a stroke.
It's likely that your stroke team will have a dietitian who can help you with any changes to your diet.
They can monitor your weight and how much you're eating and drinking, to make sure that you stay healthy. If they're worried that you're not getting everything you need, they may suggest that you take supplements or try special foods to boost your diet.
Are there treatments that can help?
Swallowing problems can get better, and most people are able to swallow safely again within the first few weeks. A small number of people have problems that last longer than this. Only a very small number of people are left with lasting difficulties.
Even if you are left with permanent difficulties, they don't have to stop you from doing what you want to do. Most people find that they're still able to live full lives despite them. But it may take some time to adjust to the changes that you need to make.
If you have problems with swallowing you should be referred to a speech and language therapist, who will work with you to try to improve it.
Your speech and language therapist will complete an assessment with you, to work out exactly what's going on. Once they know this, they'll be able to talk to you and your family about the best ways to treat or manage your swallowing difficulties. It's important that you don't eat or drink anything until your swallowing has been checked.
Your doctor or nurses may refer to you as being 'nil by mouth' until you've had an assessment this is when you're told not to eat or drink anything.
To begin with, the most important thing will be making sure that you can swallow safely. If you're not swallowing safely, it could cause infections or mean that you're not getting enough food or fluids into your body. Your speech and language therapist will explain the different things you can do.
This could include:
- Changing your diet.
- Learning techniques that can help you to swallow.
- Using aids that can help you to eat or drink more easily.
As well as these, your speech and language therapist may also get you to practise exercises to strengthen muscles in your throat, face and mouth. This may help you to swallow better and protect your airway.
Changing how you eat and drink
If you can't swallow safely, then you'll probably need to make changes to your diet with advice from a speech and language therapist.
Drinking safely
It's important to drink enough, because your body needs to stay hydrated to fight off infections and help you recover from a stroke. Water and other thin liquids are the hardest things to swallow because they're difficult to control.
Your therapist might assess you and recommend using thickened drinks to help you drink safely. These can be made using special powders to create the right level of thickness.
To make thicker liquids more enjoyable to drink, you might be able to try chilled or flavoured drinks. Making sure the drink is freshly prepared and not thicker than it needs to be could make it more pleasant to drink.
Your therapist may be able to suggest how to make some regular drinks to the right consistency, such as smoothies or milkshakes.
Eating soft or pureed food
Wiltshire Farm Foods has created a video in partnership with the Stroke Association which shows the options for soft foods, from bite-sized through to liquidised, to help you get the nutrition you need and enjoy mealtimes. If you have problems with chewing and swallowing, you may need to eat soft food. There are different categories of food softness, from soft and bite-sized through to liquidised. A speech and language therapist can advise you on the right texture.
Change the temperature
Hot foods and drinks can be difficult to swallow because you can't hold them in your mouth for long. So your therapist may suggest that you stick to cold foods, or allow hot food to cool down quite a bit before you try to eat it.
Change how and when you eat
Eating small amounts throughout the day, rather than three big meals, for example, may be better for you if you're finding it hard to concentrate or you get tired very quickly. You may also find small portions are easier to manage, or that eating earlier in the day when you have more energy, works better.
Your speech and language therapist will explain to you and your family exactly what foods are safe for you to eat. They'll also make sure that the rest of your stroke team are clear about what you can and can't eat, and how you should be eating.
Some people make a good recovery from swallowing problems. The way you eat may change over time as you go through your recovery, and you might be able to go back to eating more of the foods you are used to.
If your swallowing problems are long-term, with good care and support, you can have a good diet and enjoy your food and drink.
Swallowing assessments
You'll probably have a number of swallowing assessments while you're in the hospital, to check how your swallowing improves over time.
- Your therapist will usually begin by asking you to swallow a very small amount of water, followed by food and drinks of different consistencies, to show whether you can swallow them safely.
- A videofluoroscopy involves taking a video X-ray of your mouth and throat while you swallow. You will sit beside an x-ray machine and be given different foods and drinks to swallow. These will be mixed with a special liquid called barium that will show up on the X-rays.
- A fibreoptic endoscopic evaluation of swallowing (FEES) uses an endoscope to find out what's happening when you swallow. An endoscope is a long, thin, flexible tube that has a light and a tiny camera at the end of it. It's inserted into one of your nostrils and down your throat, so that your therapist can see how well your muscles are working and where the problems may be occurring.
You can ask for another assessment if you think your swallowing has changed. If you're not able to swallow, you'll be given fluids through a drip to make sure that you don't become dehydrated. It's also important that you get the right nutrition, so your stroke team may also talk to you about being fed by a tube.
Tube feeding
If your swallowing problems make it hard for you to eat enough, you might lose weight and miss out on important nutrients. This can cause low energy levels, and even slow down your recovery. If this happens, you might be offered tube feeding. Tube feeding means putting liquid food directly into your digestive system through a tube. This is also known as enteral feeding. You might only need it for a short time if your swallowing improves, but some people will need it for longer.
There are different types of feeding tubes. The two that are used most often after a stroke are nasogastric (NG) tubes and percutaneous endoscopic gastrostomy (PEG) tubes.
NG tubes go through the nose into the stomach. They tend to be temporary and are normally used if you'll need to be tube fed for less than four weeks. Whereas a PEG tube is inserted into the stomach through a hole in your skin. They tend to be used for longer periods.
After some time using an NG tube you are thinking of changing to a PEG, you'll need to talk through both options with your stroke team and family to decide which one is best for you. There are advantages and disadvantages to both.
Nasogastric (NG) tube
A very thin tube, not much wider than a piece of spaghetti. It goes up your nose, down the back of your throat and into your stomach.
Advantages
- Safer to insert than a PEG tube, as it's less invasive.
- Easy to remove.
- No need for sedation.
Disadvantages
- Can be uncomfortable when it's in place.
- Can fall out easily, so it may need to be replaced regularly.
- Some people don't like how it looks.
Percutaneous endoscopic gastrostomy (PEG) tubeA tube that is inserted directly into your stomach, through your skin. Advantages
- Rarely falls out.
- More comfortable.
- Can be hidden under your clothes.
Disadvantages
- More difficult to replace if it does fall out.
- You will be given a sedative when it's inserted, and a doctor or nurse will explain the risks to you.
- The area around the tube can become infected.
Tube feeding at homeIf your overall recovery is good, then your stroke team may suggest that you go home and continue the tube feeding at home. This can worry some people as they think it can be a lot to cope with. However, most people cope very well with tube feeding at home, even people who live on their own. Once you've given it a go, you'll probably find it's not as difficult as you thought.
Five reasons to consider tube feeding at home:
1. Feeding machines are usually very easy to use.
2. There's not much that can go wrong and nothing that can put you in danger.
3. You and your family will be shown exactly what to do before you go home.
4. You'll have support from community nurses once you are home.
5. You can always consider other options later, if you do find it too much.
It's up to your stroke team to make sure that you and your family have all the information, support and equipment you need before you go home. You're likely to have lots of questions, and the earlier you get the answers, the more confident you'll feel about going home.
Questions to ask before you go home
- How do I use the feeding machine?
- How do I know if the tube is in place?
- Will I still be able to eat using my mouth if I want to?
- What do I do if the tube becomes blocked?
- Do I have to clean the machine? How do I do it?
- Are there written instructions I can have?
- How do I get more food?
- Who do I contact if I have a question?
- Who do I contact in an emergency?
Although life with tube feeding can take some getting used to, it doesn't have to stop you from doing things that you want to do. Over time you'll adjust to the changes you need to make and, with a little extra planning, still be able to enjoy things like going out and going on holiday.
Who can I ask about tube feeding?
You will have individual help and advice about tube feeding in hospital and at home. Health professionals who support tube feeding include nurses, dietitians and pharmacists, but job titles can vary between areas. The main professionals who help you are:
- Dietitian.
- Specialist nutrition nurse.
- District nurse or community nutrition nurse: support at home.
- Pharmacist: help with prescriptions for feeding supplements and medications
- Speech and language therapist: advice if you are also having food by mouth or planning to go back to eating.
Tips for living with swallowing problems
Just because you have swallowing problems, it doesn't mean you can't enjoy eating. If you're missing your favourite meals and snacks, speak to your speech and language therapist or dietitian. There may be a way for you to have them, or to enjoy something similar.
Many types of everyday food are soft, or can be made in soft or pureed form. Ask your dietitian for advice about dishes you might be able to make at home and how to make them tasty and enjoyable. If you enjoy your food it can help you to get all the energy and nutrients you need to stay healthy. Soft foods don't have to be boring.
There are lots of cookery books and online recipes for tasty pureed meals. Or if you're not able to cook, there are companies that will deliver meals to you that look and taste great. Ask your speech and language therapist or dietitian if they have any recommendations.
Medication comes in different forms, including liquids, patches and inhalers. So if you're finding it hard to swallow your tablets, speak to your doctor or pharmacist to see if your medication comes in a different form that may be easier for you to take.
Always check with your pharmacist first before crushing tablets, as this can change the way some medications work and can even be dangerous.
1. Listen to your therapist
The most important thing for you to do is to follow the advice that your speech and language therapist gives you. Even though you may think that you're able to swallow safely, you can't know for sure. Not being able to eat the things you enjoy is difficult, especially when you're stuck in the hospital, or if you are feeling down. However, avoiding difficult foods, however much you miss them, will help you recover.
2. Ask questions
It's important that you understand the instructions and advice you're given, so ask your speech and language therapist to explain things again if you need them to. Don't worry if you feel that you're always asking questions. Your stroke team would much rather you ask than do something that puts you at risk. So if you want to eat something but you're not 100% sure it's OK, double-check. Or if you think your swallowing has improved, ask for another assessment, so that you can be sure.
3. Learn how to swallow safely
Although your speech and language therapist will show you, our swallowing dos and don'ts can remind you how to swallow safely.
Do
- Create time and space for you to concentrate on what you're doing. So turn off the TV or draw the curtain around your hospital bed.
- Sit up with a straight back, arms and hands forwards. If you are in a chair, keep your feet flat on the floor.
- Take your time.
- Take small amounts. Cut food up into small pieces, and just take small sips when you drink.
- Swallow twice after each mouthful, to make sure nothing is left in your mouth.
Don't
- Try to eat or drink if you're feeling tired or drowsy.
- Try to eat or drink lying down.
- Talk while you're trying to swallow.
- Use straws or cups with spouts unless your speech and language therapist has told you it's safe.
- Eat foods with a variety of textures, such as soup that has large chunks in it, or cornflakes with milk.
4. Look after your mouth and teeth
You should have help and support to look after your mouth, because the bacteria (germs) in your mouth can be breathed into your lungs. When there's a build-up of bacteria in your mouth, it raises the risk of a lung infection (pneumonia). Regularly cleaning the tiny traces of food and drink on your teeth, gums and inside your cheeks reduces the number of bacteria and lowers the risk of pneumonia. Traces of food in your mouth can also lead to gum infections or tooth decay, making your mouth sore and making it harder to eat and drink. To find out what you need to know and get practical tips, visit our guide to oral hygiene after a stroke.
If you have swallowing problems, ask your stroke nurse or speech and language therapist for individual advice about how to keep your mouth and teeth clean.
5. Talk to someone about it
Swallowing problems can be especially difficult to cope with at home. A large part of our family and social lives is about eating and drinking, so it can have a big impact when you're not able to enjoy these things anymore. Many stroke survivors feel left out when they're not able to take part in family mealtimes like they used to. Or you may not look forward to meals out, because you're embarrassed to eat in front of other people or feel awkward if you're not eating with everyone else. These feelings can take their toll. So make sure you talk to someone about them. Support groups can be helpful, because you can talk about your problems with people who are going through the same thing. But they're not for everyone, so talk to a friend or family member instead if that's easier for you whoever you feel comfortable confiding in when you're finding it tough.
Tips for family and friends
It can be difficult to know how to help someone with swallowing problems. So here are some tips to help you.
Always check
It's difficult to know what helps and what doesn't when it comes to swallowing. A straw, for example, may seem pretty harmless.However, most people with swallowing problems shouldn't use them. It should be OK to bring in food or drinks for someone in the hospital, but just double-check that it's safe with someone in the stroke team first.
Don't ignore advice
The best way to help your friend or family member is to make sure they stick to the advice they are given. You may be worried that they're going hungry or that not being able to eat is getting them down. Talking to their speech and language therapist about it should help to put your mind at ease. Together you may be able to think of something you can do to help your friend or family member feel better.
Give them time and privacy
Swallowing problems can make people feel very self-conscious. So make sure your friend or family member has some privacy when they're eating. Even if it's just pulling the curtain around their bed or asking visitors to pop out for twenty minutes while they eat. Time is also really important. Eating probably feels stressful enough for them, so rushing is only going to make it worse. So encourage them to take their time and enjoy their food.
Ask for help if you need it
Coping with swallowing problems can feel very overwhelming. So don't be afraid to ask for help. Before your friend or family member is discharged from the hospital, make sure you know who you can contact if you have a question once they're home. Talk to your GP if it's getting too much and ask what support you can get. It may also help to talk to someone else about it, especially someone who's gone through a similar situation. There will probably be a carers' group in your area or you could try your local stroke club. Dos and dont'sWhen you're helping someone to eat or drink, try to remember these simple dos and don'ts.
Do
- Make sure they're sitting up straight. A pillow may help support their trunk if they are leaning to one side.
- Allow plenty of time.
- Show them what they're about to eat, or describe it to them. Eating is just as much about how the food looks and smells as how it tastes.
- Try to present food so it looks nice, and be positive and encouraging when you offer it. Keeping food separate on the plate is much more appetising than mashing it all together. Food moulds can also help you to present pureed food nicely.
Don't
- Give them a drink or something to eat if they are feeling tired or drowsy.
- Rush them or offer too much at once.
- Move from one food to another without asking them.
- Forget that you're helping an adult, not a child.
